Disclaimer: This is purely my experience as it is happening. There are many different cancers and many different treatments, and, even for two people with the same cancer and the same drug regimen, reactions can be very different. So, what I’m going through might have very little resemblance to what you would or will or are.
Jan 29: Chemo Day 1
There was only one other person in here when we arrived at 9, by 10:30 or so the room was full (five patients; the three women all have companions with them throughout, the two men don’t). All have different stories, but I’m not yet at the stage of asking to hear them. All but one look perfectly normal – passing us on the street, you wouldn’t know anything is happening to us.
Fantastic nurse, Diana. When she first came in and saw me, she said: “Is this your first time?!?” She seemed so happy that I replied jokingly: “Don’t look so enthusiastic about it!” She explained: “I’ve been doing this [working with cancer patients] since I was in nursing school. Now that I’m near retirement, there is so much more that we can do for people.” I want to hear more of her story. I suppose there will be ample time!
She poked through my skin into the port a short, sharp, fat needle with a plastic butterfly to remove it by later. This didn’t hurt; they give you a lidocaine cream to put on the skin over the port an hour before you go for treatment. I might not have felt much anyway; the skin right over the port has little or no sensation at the moment, perhaps a small nerve was cut during surgery. I don’t like watching a big, spiky needle get shoved into me, but I couldn’t feel it.
I wore a low-cut shirt on purpose, so there was no need to undress any part of me, as you can see in the photo above.
Via the IV tube into the port, Diane first administered one syringe of an anti-nausea med (Aloxi – sounds plausible as a girl’s name), then dripped in two different steroids, again to control nausea. All this was merely preparation, and took about an hour total.
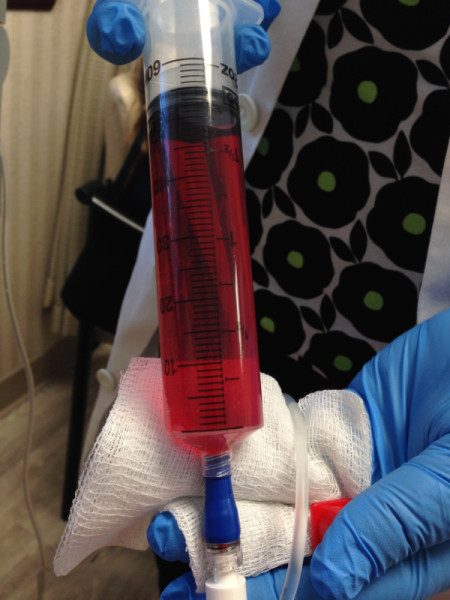
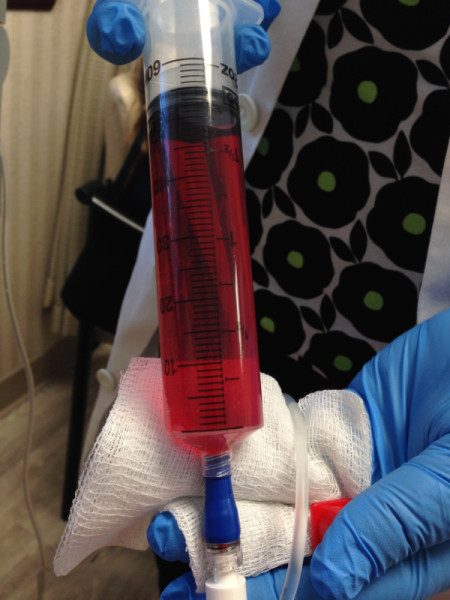
She then pushed in 50CC of adriamycin, aka doxorubicin, which for some reason had to be done slowly but by hand. Then followed a saline drip, before starting 1000mg of cytoxin, which she timed to last 75 minutes to make it a little easier on me the first time around. Numerous times during these hours I had to go pee, and so did the other patients. All that fluid being pushed into us needed an outlet.
During Infusion
They call it infusion. We’re being steeped in poisons, really. Some side effects are immediate:
- A metallic taste in the mouth, slightly noticeable during the chemo drips.
- A nasty chemical taste in mouth, instantaneous but brief, during the heparin injection done at the end to clear out the catheter and prevent clots.
Other than that, nothing particularly noticeable during. We hopped on the wifi from our laptops, looked at work and other stuff, I took notes on the process. I tweeted.
We came home, and I ate a hearty lunch, drank milky tea (yay, my Scottish Breakfast tea arrived from Amazon yesterday). After that I felt very sleepy. Maybe I should nap now as Diane told me I might feel wired later from the steroids.
4pm headache – dehydration? some body aches, which I had before, possibly from lack of physical activity. Hope I didn’t catch a bit of flu before. Can’t think what else explains the persistent body aches.
I’m supposed to stay well hydrated, at least 2 liters of water a day (I drink more than that most days already). One of the side effects of chemo is dry mouth, so I’ll undoubtedly want to. But then I’ll be waking up even more often at night to pee…
6:30 pm (~8 hours after first chemo) Began to feel first twinges of nausea, took odansetron (Zofran). That’s the more powerful of the two anti-nausea pills they gave me, it’s supposed to be good for 8 hours, the other for 4, but I can take them at 4-hour intervals.
Blood pressure 116/72 (cheap home BP meter). It was 130/something yesterday during my pre-chemo doctor visit. The lower level is what used to be normal for me, before I got a cancer diagnosis. Did a bit of seated yoga stretching of my hips – too much sitting around lately. 7:40 I don’t feel nausea (odansetron works fast! yay!) but I don’t have much interest in food right now, either. Slight burning sensation/taste in the back of my mouth. 9:00 hot bath to help with the muscle aches and headache (a side effect of any of several of the drugs), seems to have worked. Now just very tired, but will stay up until 10:30 to take the other nausea drug.
Jan 30 Chemo Day 2
Went back for the Neulasta shot in the afternoon (have been taking Clarityn, which is known to alleviate the bone pain from this, though apparently no one knows why). Brendan drove – I was way too foggy and out of it to be safe driving.
From Rick, email: “Something I read once that was useful to me: The trite expression about ‘fighting cancer’ misses the mark subtly but fundamentally. The actual truth is that you are the battleground in which cancer gets fought. You are not a soldier. Flattering you by implicitly calling you one is just a category error, and helps nobody.”
I’ve read elsewhere words to the effect of: “Don’t talk about my ‘brave battle’, because, if I die, that will make me a loser.”
Agree on both.
Today have eaten one small apple, one banana, blueberries with vanilla yogurt, and a slice of chocolate cake (30 mins or so ago). Now heartburn. Chewing gum worked a bit, but I ended up going out to buy antacid tablets – something I’ve never had any need for up to now.
8ish Ate rice with olive oil and slivers of parmesan. So far, so good.
A couple of brief but irresistible naps during the day. Trying to drive myself to get the Neulasta shot would have been a bad idea.
Jan 31 Chemo Day 3
No more nausea (so I stopped taking either pill) since about 28 hours after first chemo administration.
Felt good this morning, started doing some work even, then got distracted by this and that. Mentally don’t feel all there.
Meena came by to bring me dal and veggies, which proved to be divine for dinner with rice from the new rice cooker.
In the evening, bone pain from the Neulasta makes itself felt.
Nose feels weird – numb inside and drippy. Apparently I’ll also lose my nostril hairs, which will mean a constant nasal drip. Chemo leaves us very little dignity.
Feb 1 Chemo Day 4
Very sleepy some of the day. Worst symptom at the moment is constipation. The literature says that chemo can cause that, or diarrhea, or both in succession (in either order). So I didn’t know what to treat for, especially having had both recently, including a couple of severe cases of diarrhea (one due to food poisoning in Port Douglas, the other back at home, origin unknown). Took Colace.
Feb 2 Chemo Day 5
Skin/scalp becoming heat-sensitive. Yesterday I wanted to sit in the sun on the balcony, but even with sunscreen on, it felt like my exposed skin was burning immediately. This morning my head was sensitive both to hot water in the shower and the hair dryer.
Ears ringing
At least I’m managing to shit a bit.
Didn’t get enough sleep last night, then slept for maybe an hour in the middle of the day. Now feel jet-lagged, don’t have my usual sense of how much time is passing or what time it is.
Feb 3 Chemo Day 6
Sinus infection coming back (I should have known: depression is a symptom!), have a call in to Dr J about this. (His assistant called back later with a prescription – same antibiotic I took just before chemo for the same infection. If this doesn’t knock it out, I’ll have to drag myself up to the city to see him and get a culture.)
Sleep even worse than what used to be normal for me, then I had to get up for meetings so only slept 11:30pm-5:30am. After a few solid hours of work in the morning, I felt sluggish and unproductive most of the day. It’s possible that I’m too hard on myself about work.
Tea with milk was too hot and harsh, didn’t finish it. Maybe coffee with milk so it gets colder?
Turned the shower way colder than usual, too. Don’t feel quite as burned afterwards as I did yesterday.
Tired, dizzy, tightness/pain in the pit of my stomach. Ate, but that doesn’t seem to have changed anything. I don’t have fever, but I feel hot. At the moment, feet are icy and hands are hot. Other times, both are icy.
(I ended up taking anti-nausea medication again, but it makes me drowsy and stoned.)
Rossella’s flight from NYC was delayed seven hours (due to a medical emergency on the plane before it even got to New York). I ordered food from Munchery to be ready for her; I didn’t have the energy to cook.
Feb 4 Chemo Day 7
Slight bleeding in bladder? and slightly bloody stool. Nausea in the morning, took chlor…, which made me drowsy and stoned for a few hours. Napped 4-5, went to sleep again at 11:30pm.
Feb 5 Chemo Day 8

Woke up at 6:30, felt almost normal til about 11:30. Ate bacon and oatmeal for breakfast ~9am. Maybe I’m hungry now? Ate. Not much help. I feel completely flattened now. 3 loads of laundry probably didn’t help.
Feb 6 Chemo Day 9
Still a bit tired from sinus infection or whatever, but I had a productive work day, which made me happy. My colleagues are working to make me feel included and useful, and I think I’m actually being useful, all of which is a huge morale booster.
Nasty stuff coming out of my sinuses. Not sure if the slight sore throat is related to that, or to chemo, or I’m getting a cold. My propensity to get respiratory infections is not at all helpful in chemo. I’m trying to be very careful about exposure, but of course it’s hard when you spend physical time with people who may be exposed to just about anything at work, school, etc. But it would be just as unhealthy for me not to see anybody at all.
Feb 7 Chemo Day 10
If it weren’t for the sinus infection that came roaring back (I took antibiotics for it just before starting chemo), I might feel just about normal now. Except I still can’t eat much in one sitting, and I still get some acid reflux regardless of how little I eat.
I am losing weight already, down maybe 3 pounds since chemo started. This may also be attributable to having absolutely no interest in alcohol, and not much in sweets.
So far hair is still there, though the texture seems different, drier maybe. It’s long past the point where I would normally have had it cut, so it’s also lank and shapeless but… why bother now? It seems that I can expect it to start falling out in clumps right about day 14.
Feb 9 Chemo 1.11
Very interrupted night’s sleep, as those before – I keep waking up because my mouth is uncomfortably dry, then I have to pee because of all the water I drink. Will borrow a humidifier to see if that helps. Eyes also get dry.
Feb 10 Chemo 1.12
Hair starting to fall out more than usual, though not yet in clumps.Accompanied by a slight burning sensation in my scalp, though I may be imagining that.
Feb 11 Chemo 1.13
Maybe the sinus infection is going. Still fatigued and depressed, but it’s hard to know how much of that is emotional.
Trying to get my digestive system ready for next round of chemo by eating lots of fiber. This achieved a brief bout of diarrhea. Sigh.
Blood work and pre-chemo visit with Dr L. White cell count actually higher than he wanted, probably due to the infection, so the Neulasta dose will be halved this week. I seem to be tolerating everything pretty well, so… on we go. Weighing confirmed I have lost 3 or 4 pounds.
In the waiting room I talked with a woman who has had two cancers (the first must have been when she was very young); she was awaiting results on tests. She taught school for 35 years, and kept up her teaching schedule through chemo over 20 years ago, when it was a lot harder (no anti-nausea meds). While raising small kids. So… it is possible.
Hair starting to come out, a bit at a time, all over my body.
my breast cancer story (thus far)