…continuing the story from How I Knew I Had Cancer…
While I was still in Paris, the initial pathology report was emailed to me, but I didn’t understand much of it. I bought Dr. Susan Love’s Breast Book from Amazon (an expert friend had recommended it when my mother-in-law had breast cancer in 2001), downloaded it immediately on my Kindle, and began reading it sporadically.
It’s somewhat creepy that Amazon and Google knew what was going on with me long before almost anyone else did. Amazon started recommending books on chemotherapy, until I removed Dr Susan’s book from my “recommend based on” list. I did not need that reminder every time I opened Amazon.
I decided immediately not to read the section of Dr. Love’s book on causes and risk factors. I have cancer, it’s a done deal. There is no point in beating myself up over “Should I have done this or not done that?”
I later learned that:
“The most significant risk factors for breast cancer are gender (being a woman) and age (growing older).” breastcancer.org
I can’t help either of those things, so… I won the lottery: I’m one of the “About 1 in 8 U.S. women (about 12%) [who] will develop invasive breast cancer over the course of her lifetime.”
Nov 7: Took the train from Paris to London and then to Milton Keynes to visit my stepmother Ruth, whom I hadn’t seen since my dad’s funeral in 2011. Spent the weekend jabbering nervously, but at Ruth’s suggestion I did not do much “homework” about my cancer just then.
Nov 10: Flew from Heathrow to SFO. I began to read Dr Susan Love again almost as soon as I sat down on the plane. I took another look at the pathology report on my laptop, now that I had enough information to begin to understand the implications. Which weren’t great. I was terrified. I had never expected to live to be very old, but… it’s way too soon to die now. Will I be able to do all the things that I had just, cautiously, begun to hope I might?
When in-flight service finally began, I bought and downed two bourbons in quick succession. Watched three movies. Couldn’t sleep. In a torment of fear, rage, misery. Finally got home.
Nov 11: I went to the mammography office to pick up all the imaging and pathology reports.
In the evening I saw Dr Valerie Traina, the surgeon recommended by the gynecologist I still haven’t even met yet. She confirmed what I thought I’d understood from the reports: this is a “fairly aggressive” tumor.
Because most cancers in pre- or peri-menopausal women are hormone-sensitive (grow faster in the presence of hormones), as later proved to be true of mine, she told me to immediately stop all hormones. Joy. This means I can look forward to suddenly, on top of everything else, dealing with all the menopause symptoms that I was taking hormones to control: headaches (sometimes migraines), sleeplessness, hot flashes.
Nov 12-15: Attended USENIX LISA in Seattle, a chance to catch up with the sysadmin / devops sector of the tech industry. Saw a lot of people I know, met some new ones, talked and listened a lot. I felt dazed a lot of the time, only partly due to jetlag.
random thoughts ~Nov 15-17: I’ve joined a sisterhood I never wanted to be part of.
I’m frightened. “Fairly aggressive”. What does that even mean? I read Dr Susan Love’s Breast Book, but it’s overwhelming. My brain shuts down – too much information.
I’m walking into a country I don’t know. Usually this would excite me – I love new places. This time I’m terrified. And I’ll be in this country for the rest of my life.
So many clichés. Brave battle. Victim.
I don’t want my life to be reduced to this.
So tired.
Another phrase I forbid anywhere near me: Raising awareness.
I am fucking aware of cancer. I was aware long before it happened to me. Hardly anyone in the world needs to be any more aware than they are.
Nov 17: Had an MRI to pinpoint where the tumor is, see if there might be any others (there weren’t). Once again lying face down with my breasts dangling through holes in a table. 30 minutes total. Then an EKG, urine and blood samples to ensure that I was ready for surgery. I asked the EKG technician if it all looked ok. “I’m not allowed to tell you, but if something was wrong, I’d be calling for help, not chatting with you. I can say that it’s as if you studied for this test.” At least one part of me is working well.
Nov 18: Slept ok, but very tired. Not sure if I’m tired because I’m emotionally overwhelmed, or vice-versa, or both. Plus I’m probably getting a sinus infection, which won’t help anything.
But the DMV goes on, and having cancer does not excuse me from dealing with banalities like needing to renew my driver’s license.
I’m trying to do my homework: reading Dr Susan Love’s Breast Book, and breastcancer.org, trying to absorb a lot of very complex information about what is happening to me, and what might be done to me. It makes me tired very quickly. My brain doesn’t want to deal with this. I want it to just NOT be happening. But I never get those choices, do I?
I don’t know enough right now to make decisions. But I fear I will never know enough. And the wrong decision could be fatal – or more quickly fatal than some other decision.
This is a life-shattering event. Of the dreams I was cautiously beginning to dream, I don’t know what I may still be able to aspire to.
I’ve been public about some of the traumas of my life to date, and very private about others. I have no idea as yet how or even if I want to talk about this in public. Some people ie my colleagues need to know so that they won’t be let down if I can’t make or deliver on work commitments. Friends and family deserve to know. But there are so many labels and boxes I don’t want applied to me.
I do and don’t want to talk about it. I want to scream and cry. My heart is pounding. My head hurts.
Nov 24: As part of “getting my shit together,” in case of unexpected complications, I went to SF to see my lawyer and sign docs: a living will (AKA advanced health directive), and a will will (the kind you need if you die). All of this in a fat, green, faux-leather “Estate Planning Portfolio,” which makes my estate look much more impressive than it is.
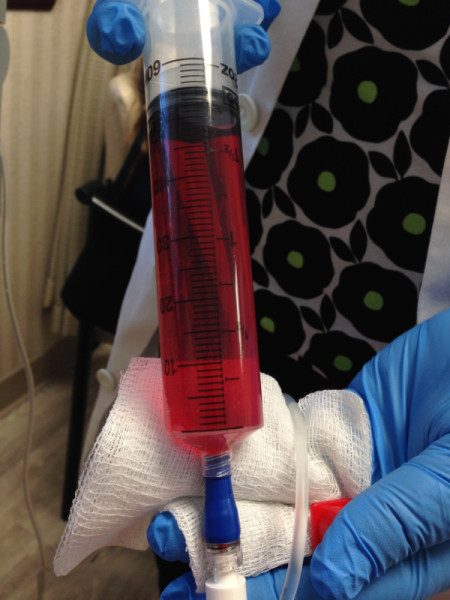
Nov 25: Surgery
my breast cancer story (thus far)