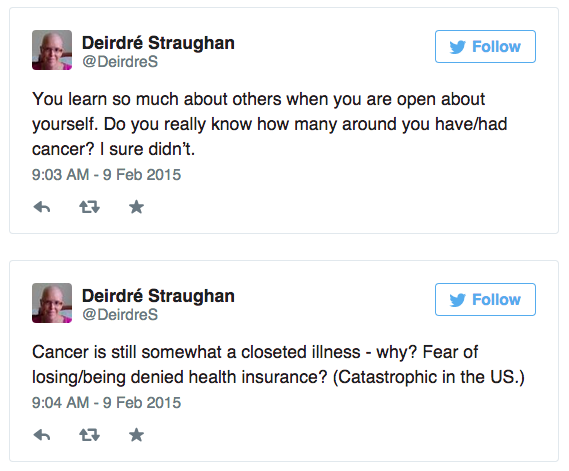
You learn so much about others when you are open about yourself. Do you really know how many around you have/had cancer? I sure didn’t.
— Deirdré Straughan (@DeirdreS) February 9, 2015
Cancer is still somewhat a closeted illness – why? Fear of losing/being denied health insurance? (Catastrophic in the US.) — Deirdré Straughan (@DeirdreS) February 9, 2015
The idea that you can prevent or cure cancer via diet and exercise is part of this victim-blaming. You didn’t do the right things!
— Deirdré Straughan (@DeirdreS) February 9, 2015
Continuing from Chemo, Round 1:
I will soon be able to shave my legs with a lint roller. (See! I’m looking at the bright side!) — Deirdré Straughan (@DeirdreS) February 11, 2015
Feb 12 Chemo 2.1
Chemo round 2 (eventually I’ll stop counting).
— Deirdré Straughan (@DeirdreS) February 12, 2015
(No, I didn’t.)
Why Everyone Seems to Have Cancer http://t.co/RDBYdiEvYq (just not quite so early in life – I’m often the youngest person around here) — Deirdré Straughan (@DeirdreS) February 12, 2015
Started the day with a blistering headache, took 2 ibuprofen at home. It was finally fading when the chemo started, but now the headache from aloxi has started.
While pushing the adriamycin, the nurse said “Tell me if anything feels painful or burning.” It didn’t, but I could sorta feel (or imagined I did)… something. Like being aware of my blood rushing around my veins and arteries.
8:45pm – not quite nausea, over-full from eating a bacon and avocado sandwich Ross made for dinner. Dizzy, terrible headache.
Useful thing to have when you’re doing chemo: a Dyson pet model vacuum cleaner.
— Deirdré Straughan (@DeirdreS) February 12, 2015
So far I’m just getting individual hairs falling out, but more of them than usual, and increasing. Like a rainstorm just starting. — Deirdré Straughan (@DeirdreS) February 12, 2015
Apparently it will be different from my current hair, at least the first growth. We shall see… some months hence.
— Deirdré Straughan (@DeirdreS) February 12, 2015
Mini humidifier runs all night on a 1.2 liter bottle, alleviates dry mouth from chemo so I sleep a bit better. pic.twitter.com/HrBRCYyPxt — Deirdré Straughan (@DeirdreS) February 13, 2015
My hair is longer than usual because I figured no point in cutting it now. Long blonde hairs everywhere. Ugh.
— Deirdré Straughan (@DeirdreS) February 13, 2015
“Cancer is not a concentration camp, but it shares the quality of annihilation: it negates the possibility of… http://t.co/rwuI2Y7XFc — Deirdré Straughan (@DeirdreS) February 13, 2015
Feb 13 – Chemo 2.2
Slept ok, woke up around 4am, took Zofran, read a while, then slept til 8:45 weight up to 149 from 143 a few days ago, but that may be water retention and/or constipation ate a little yogurt with flax seeds, then boiled potatoes with a few anchovies for lunch mostly just tired/groggy 7pm – stomach acid ramping up again 8pm – constipated. ate dinner, not a bit of intestinal cramps
If you want to know the nitty-gritty of what chemo is like (for me, so far), here’s a diary of Round 1 http://t.co/I2CIzk0yBx — Deirdré Straughan (@DeirdreS) February 14, 2015
(If you don’t want to know the nitty-gritty of chemo, that’s ok too! Everyone has a right to their own nitty-gritty threshold.)
— Deirdré Straughan (@DeirdreS) February 14, 2015
Feb 14 – Chemo 2.3
Acid stomach, slight (so far) headache, which could be seasonal allergies – lots of pollen around today, and, sadly, cancer doesn’t give me a pass on any of my normal physical ailments. 1:15pm – spine feels bruised, stomach acid and/or nauseous
So this is the part of the cycle when the Neulasta results in feeling like the knobs of my spine are all bruised. — Deirdré Straughan (@DeirdreS) February 14, 2015
couldn’t stand my legs anymore, shaved them. carefully [Because chemo knocks down your immune system, you have to be extremely careful of any possible sources of infection, including even minor injuries, like shaving cuts.]
“knowing another has leprosy makes our cancer none the easier to bear.” http://t.co/cMMQkozCZ2
— Deirdré Straughan (@DeirdreS) February 14, 2015
Crushing waves of fatigue. Well isn’t this fun. — Deirdré Straughan (@DeirdreS) February 14, 2015
Wish I’d cut my hair very short before it started falling out. Shedding like a retriever is gross and annoying.
— Deirdré Straughan (@DeirdreS) February 15, 2015
I think tomorrow might be time to buzz my hair off – what’s left of it. I feel… sick. — Deirdré Straughan (@DeirdreS) February 15, 2015
Apparently my body thinks it’s very tiring to shed hair.
— Deirdré Straughan (@DeirdreS) February 15, 2015
Feb 15 2.4
Woke up this morning from a dream that I was crying for my hair, and crying for Jon Stewart. Smells can be overwhelming, and some that were previously pleasant now are not. Whole Foods was a weird sensory experience. Then rice cooking in the cooker brought me close to vomiting (took a pill, in fear that real nausea would set in). After I spent all day being annoyed by long strands of hair going everywhere, Brendan used the clippers (#7, then #3 for cleanup) to buzz my hair off very short. I’ve had hairstyles almost this short in the past, so it’s not so much of a shock at the moment, but visibly thinning – scalp is very visible when it’s wet. And my head gets cold. Leg hair is growing back much more slowly than usual.
Feb 16 2.5
am Feeling sickish and a bit dazed. eating was somewhat difficult today 11pm – feeling slightly nauseous – that got worse before I finally went to sleep, ended up taking a pill
Back to the “food is difficult” stage. Last night the smell of rice (!) made me nauseous. Today it’s just about any food smell at all. — Deirdré Straughan (@DeirdreS) February 16, 2015
Can’t say I really recommend the chemo weight loss plan, but it is effective.
— Deirdré Straughan (@DeirdreS) February 16, 2015
Hair chopped short and/because it’s increasingly falling out. How long to full bald? pic.twitter.com/vkFt1qc1yG — Deirdré Straughan (@DeirdreS) February 17, 2015
Oh, so apparently I should be playing scrabble during chemo: http://t.co/IfWePafDvq (but I’d win anyway!)
— Deirdré Straughan (@DeirdreS) February 17, 2015
Here’s the rub: “The only way to know if it worked…” http://t.co/gdVHhRfbDW — Deirdré Straughan (@DeirdreS) February 17, 2015
Feb 17 2.6
could not eat or even have tea or coffee til late in the morning, eventually had a bit of yogurt, then lunch (chicken), a couple more light meals during the day. This evening it was hard to figure out what I could cook and eat that didn’t make me queasy even to think about
This bolt-out-of-the-blue I’m about to vomit feeling… I could do without that. Also the sudden chills to the head.
— Deirdré Straughan (@DeirdreS) February 17, 2015
Time for the “What food won’t make me want to heave tonight?” game. I hate this so much. — Deirdré Straughan (@DeirdreS) February 18, 2015
Feb 18 2.7
Woke up at 6:30, feeling almost normal. Fingers crossed.
By 11, have had only a cup of coffee with milk and a bit of vanilla yogurt. Stomach very acid. Trying to find something more substantial I can face eating. Biscuits?
Baldish patches appearing at the sides of my head, I guess hair is rubbing off when I sleep (on my side). Hair all over the place. Vacuum.
— Deirdré Straughan (@DeirdreS) February 18, 2015
Swallowing is a bit hard. Have to hold things in my mouth and think about it. Going to SF to see Dr J today, to get a sample of the gunk in my sinuses since the infection certainly is not going away. pm – That was exhausting.
After eating very little today, made homemade cream of broccoli soup that I could eat. Trick now is not to gorge – so hungry! — Deirdré Straughan (@DeirdreS) February 19, 2015
Feb 19 2.8
There are times when the awareness of mortality hits me hard http://t.co/A58IW6PanY
— Deirdré Straughan (@DeirdreS) February 19, 2015
Once again at the stage of probably would feel pretty normal, except for this damned sinus infection. Awaiting culture results. Thankful for Dr J.
Things I probably won’t need to spend money on this year: hairstyling, or any form of depilation. — Deirdré Straughan (@DeirdreS) February 19, 2015
BTW folks, when you hear someone has cancer? Don’t blame them. It’s inhumane and unhelpful (no, not happening to me) http://t.co/qOhTNIgI0B
— Deirdré Straughan (@DeirdreS) February 19, 2015
There is enough stigma around cancer in general without that kind of crap. — Deirdré Straughan (@DeirdreS) February 19, 2015
Feb 20 2.9
Oh, just sitting around going bald, how about you? (Also: really awkward to take a photo of the top of my own head.) pic.twitter.com/Ho74TXtEge
— Deirdré Straughan (@DeirdreS) February 20, 2015
Sigh. Really not helpful to have a sinus infection during chemo. And chemo makes it hard to get rid of any infection. — Deirdré Straughan (@DeirdreS) February 21, 2015
My daughter fwded this. Offers a good way to think about wig vs bald look question for chemo patients http://t.co/aQ6eVfPdJJ – and funny/sad
— Deirdré Straughan (@DeirdreS) February 21, 2015
Dr J’s assistant called with the news that there’s staph in my sinus. Waiting for the next round of antibiotics to be ready at Walgreens.
Feb 23 2.12
The French way of cancer treatment http://t.co/S5Bb4jjs9m via @Reuters (NB: I’m getting very good care in Los Gatos.) — Deirdré Straughan (@DeirdreS) February 23, 2015
I somehow feel that I should not have to be the one who removes considerable quantities of my own hair from the Dyson. It’s a bit depressing
— Deirdré Straughan (@DeirdreS) February 23, 2015
Thanks to Celeste and @dpp for weekend visits to keep me company, with delicious dinner and Heidi’s pies! — Deirdré Straughan (@DeirdreS) February 23, 2015
@rad_rahman Sadly, Jobs later limited his own lifespan by making stupid decisions about cancer http://t.co/1OLK1H3TfJ
— Deirdré Straughan (@DeirdreS) February 24, 2015
If it wasn’t for the sinus infection, I’d feel ok at this stage in the chemo cycle. But chemo is making it v hard to treat the infection. — Deirdré Straughan (@DeirdreS) February 24, 2015
Started cefuroximine Saturday. Immediately realized that taking it with a small food or even large smoothie is not sufficient to stave off the nausea that it induces – has to be a full meal. Which will be tricky after this week’s chemo, though I guess I can keep using the anti-nausea drugs.
Have lots of work to do, deadlines that must get done. This will be hard this particular week.
Feb 24 2.13
Annoying difficulties in regulating body temperature. Don’t know if that’s chemo or near-baldness.
I keep thinking I should/do have more energy. Very frustrated when it turns out I don’t.
— Deirdré Straughan (@DeirdreS) February 25, 2015
Feb 25 2.14
Taking an antibiotic which I know adversely affects my mood. Unfortunately, knowing why I’m depressed doesn’t actually prevent feeling it. — Deirdré Straughan (@DeirdreS) February 25, 2015
Fighting drug-induced blues, and dreading another round of chemo.
— Deirdré Straughan (@DeirdreS) February 26, 2015
My naturally multicored hair seems to be falling out selectively, darker hairs first. I’m suddenly very blonde (what’s left). — Deirdré Straughan (@DeirdreS) February 26, 2015
Drove myself to Dr L for my pre-infusion blood test and consult. On we go.
Appetite has been good the last few days, so my weight there (fully clothed) is 148.
Asked about a few things:
- Yes, bruising and wounds on my forearms are again due to steroids. He will halve the dose next time since I seem to be doing fine controlling the nausea, may not need as much.
- Taxol infusions will each take longer than AC, he says. And will be weekly. On the upside, I won’t have to return for Neulasta shots.
- Common side effect of Taxol is itching and hives. Thrilling. [Never got this, except a rash around my forefingers and thumbs for a week or so – seemed more like a contact dermatitis, but I couldn’t think of anything I had gripped in both hands that way.]
Feb 26 – Chemo 3.1
Come Healing of the body, come healing of the mind http://t.co/PhEKESKHGJ
— Deirdré Straughan (@DeirdreS) February 26, 2015
Aloxi and 2 steroids in, feeling a bit dizzy and sick.
Chemo 3 done, now at the “drugs make me stoned, steroids make me want to eat everything in sight” stage. Bought more hats. — Deirdré Straughan (@DeirdreS) February 26, 2015
BTW, if you want to do something for breast cancer, donate to Planned Parenthood so that every woman can get screened.
— Deirdré Straughan (@DeirdreS) February 26, 2015
TIL that chemo upsets the body’s temperature regulation. Actually, had kinda figured that out already. And it’s not just the lack of hair. — Deirdré Straughan (@DeirdreS) February 27, 2015
So I bought a rice cooker, and now I can’t stand the smell of rice. #chemoproblems
— Deirdré Straughan (@DeirdreS) February 27, 2015
Now at “if I smell food I will be sick” stage. But have to get enough food down me to take this antibiotic with. Can I just sleep for 6 mos? — Deirdré Straughan (@DeirdreS) February 27, 2015
9pm – still have the aloxi headache
Feb 26 – Chemo 3.2
Not doing very well on scheduling tweets today for my monthly roundup, so some things I meant for later coming in today. Blame the meds.
— Deirdré Straughan (@DeirdreS) February 27, 2015
my breast cancer story (thus far)